Netrin-1 blockade inhibits tumor associated Myeloid-derived suppressor cells, cancer stemness and alleviates resistance to chemotherapy and immune checkpoint inhibitor
Abstract
Drug resistance and cancer relapse represent significant therapeutic challenges after chemotherapy or immunotherapy, and a major limiting factor for long-term cancer survival. Netrin-1 was initially identified as a neuronal navigation cue but has more recently emerged as an interesting target for cancer therapy, which is currently clinically investigated. We show here that netrin-1 is an independent prognostic marker for clinical progression of breast and ovary cancers. Cancer stem cells (CSCs)/Tumor initiating cells (TICs) are hypothesized to be involved in clinical progression, tumor relapse and resistance. We found a significant correlation between netrin-1 expression and cancer stem cell (CSC) markers levels. We also show in different mice models of resistance to chemotherapies that netrin-1 interference using a therapeutic netrin-1 blocking antibody alleviates resistance to chemotherapy and triggers an efficient delay in tumor relapse and this effect is associated with CSCs loss. We also demonstrate that netrin-1 interference limits tumor resistance to immune checkpoint inhibitor and provide evidence linking this enhanced anti-tumor efficacy to a decreased recruitment of a subtype of myeloid-derived suppressor cells (MDSCs) called polymorphonuclear (PMN)-MDSCs. We have functionally demonstrated that these immune cells promote CSCs features and, consequently, resistance to anti-cancer treatments. Together, these data support the view of both a direct and indirect contribution of netrin-1 to cancer stemness and we propose that this may lead to therapeutic opportunities by combining conventional chemotherapies and immunotherapies with netrin-1 interfering drugs.
Introduction
Netrin-1 is a multifunctional, secreted, laminin-related glycoprotein that plays key roles in neuronal navigation, angiogenesis, and cell survival [1,2,3]. Netrin-1 is also implicated in numerous pathologies including type 2 diabetes, cardiovascular disease, and cancer [4,5,6,7,8,9]. Its activity has been shown to principally occur through the regulation of the signaling pathways transduced by its main receptors, Deleted in Colorectal Carcinoma (DCC) and UNC5-Homolog (UNC5H- i.e., UNC5A, UNC5B, UNC5C, UNC5D) [10, 11]. Notably, netrin-1 has been shown to be up-regulated in many tumor types, and this up-regulation has been proposed to act as a selective mechanism that blocks apoptosis induced by the dependence receptors DCC and UNC5B [4, 12].
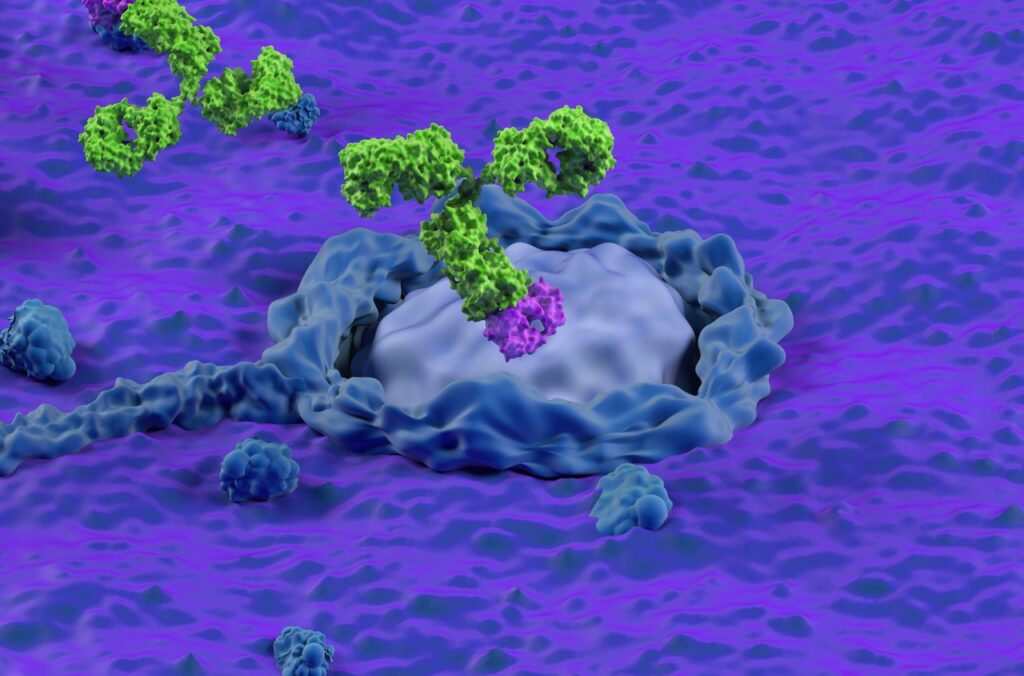
Efforts to develop drugs that inhibit the interaction of netrin-1 with its receptors have therefore been initiated. Several pre-clinical proof-of-concept studies have highlighted that candidate drugs interfering with netrin-1-receptor interactions markedly inhibit tumor growth and metastasis [13,14,15,16]. NP137, an anti-netrin-1 targeted monoclonal antibody strongly accumulate within netrin-1 expressing tumors and was recently evaluated in a phase I clinical trial among patients with advanced solid cancers [17, 18]. Interim results included both excellent safety profiles and encouraging signs of clinical activity, particularly for gynecological indications [19]. Benefits were seen in patients despite highly advanced disease resistant to standard of care, including chemotherapies and immune checkpoint inhibitors [20, 21].
A common view is that resistance to these anti-proliferative drugs is intrinsically linked to the presence of Cancer Stem Cells (CSCs) or Tumor-Initiating Cells (TICs) within the tumors. The notion is that CSCs and TICs rely on the existence of a distinct subset of tumor cells that possesses the capacity to sustain tumor growth [22]. CSCs/TICs are thought to express specific markers at the cell surface and are identified functionally based on their ability to propagate tumors when serially transplanted into recipient mice [23]. Whether CSCs are a distinct subset of cancer cells, or whether they represent a functional state of some cancer cells, remains a matter of debate. To date, the general consensus is that CSCs are key to clinical progression due to their ability to self-renew and resist chemotherapies or more recently to immune checkpoint inhibitors [24,25,26,27,28], thereby facilitating tumor relapse [29].
In the present study, we thus investigated netrin-1 implication in breast and ovary cancer and its putative link with cancer stemness and resistance to chemotherapy/immunotherapy. We show that netrin-1 expressed by cancer stem cells promotes resistance to anticancer drugs. We also associate netrin-1 expression with clinical progression and demonstrate that in various animal models, netrin-1 interference selectively impacts CSCs/TICs, thus potentiating sensitivity to chemotherapy and anti-CTLA-4 monoclonal Antibody (mAb) immunotherapy. Finally, we describe the integration of netrin-1 within the tumoral microenvironment and show that the anti-netrin-1 mAb inhibits tumor recruitment of a subtype of myeloid-derived suppressor cells (MDSCs) called PMN-MDSCs. We provide functional evidence that these immune cells promote the CSC phenotype, and consequent resistance to anti-cancer treatments.
To read the rest and the results, click on the following link: